To revolutionize care delivery, wearable health devices must be more than gadgets. Since the advent of fitness trackers in 2009, wearable devices that collect health information have flooded the digital market. As it stands, recent data shows that 33% of consumers stopped using their wearables after 6 months, and 50% stopped using it in a year. Many have speculated that wearable devices are simply a passing health fad or another tech gimmick. While standalone wearable devices may not do much to change healthcare, those that are coupled with evidence-based mobile apps have the capacity to facilitate healthcare’s ongoing transformation.
In a three part blog series, we will examine how mHealth’s convergence with wearable health technology will, and in some cases already is equipping patients as well as healthcare and insurance providers to achieve improved health outcomes.
Wearable Health’s Forthcoming Impact on Providers
As more healthcare organizations transition to value-based care, many are beginning to test mobile wearable health solutions, largely for remote patient monitoring purposes. Such solutions allow physicians and clinicians to remotely oversee patients during treatment visits, when administering medication, or pre- and post-operations. Doctors could more informedly determine how patients are responding to treatments or recovering from procedures, regardless of whether their patients are in outpatient, inpatient or home settings. With this enhanced set of data, more personalized treatment plans can be delivered to patients.
Wearable health devices are capable of tracking medically useful health information that can support physicians and clinicians in detecting serious medical conditions at an early stage.
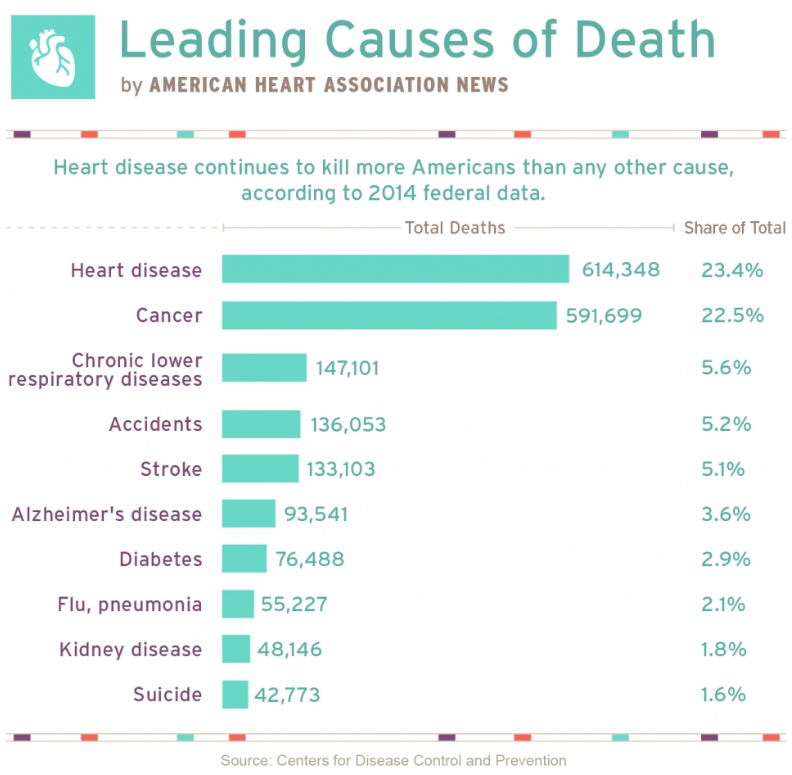
For instance, wearable health solutions that measure physical activity and sleep patterns can unlock data that was once inaccessible to doctors. Heart rate readings collected during periods of sleep can enhance physicians’ ability to identify patients’ risk of having a heart attack. Abnormal elevations and fluctuations in heart rate also correlate with medical conditions such as obstructive sleep apnea. In this case, wearable health solutions can support physicians in identifying undiagnosed heart disease sufferers, and lower the financial burden of heart attack and stroke on insurers and patients.
Wearable health solutions that integrate patient health information (PHI) including health condition, treatment plan and prescription data with sensor-generated data can further be integrated into the care process. While patient-facing mHealth apps deliver relevant suggestions for self-care and disease management, clinician-facing apps can flag potential health issues and deliver alerts to providers. Such solutions will need to be HIPAA compliant and prevent physicians from experiencing data overload.
Hospital-assigned wearable health solutions with GPS capabilities can even support hospital staff in protecting patient safety. The devices could deliver warnings to patients who enter contaminated areas, surgery rooms or other hospital areas that are off limits, and generate alerts for hospital staff. These solutions could also alert clinical care teams of instances of patients wandering outside of the hospital before being discharged.